
Breaking News
 IT'S OVER: Banks Tap Fed for $17 BILLION as Silver Shorts Implode
IT'S OVER: Banks Tap Fed for $17 BILLION as Silver Shorts Implode
SEMI-NEWS/SEMI-SATIRE: December 28, 2025 Edition
 China Will Close the Semiconductor Gap After EUV Lithography Breakthrough
China Will Close the Semiconductor Gap After EUV Lithography Breakthrough
 The Five Big Lies of Vaccinology
The Five Big Lies of Vaccinology
Top Tech News
 EngineAI T800: Born to Disrupt! #EngineAI #robotics #newtechnology #newproduct
EngineAI T800: Born to Disrupt! #EngineAI #robotics #newtechnology #newproduct
 This Silicon Anode Breakthrough Could Mark A Turning Point For EV Batteries [Update]
This Silicon Anode Breakthrough Could Mark A Turning Point For EV Batteries [Update]
 Travel gadget promises to dry and iron your clothes – totally hands-free
Travel gadget promises to dry and iron your clothes – totally hands-free
 Perfect Aircrete, Kitchen Ingredients.
Perfect Aircrete, Kitchen Ingredients.
 Futuristic pixel-raising display lets you feel what's onscreen
Futuristic pixel-raising display lets you feel what's onscreen
 Cutting-Edge Facility Generates Pure Water and Hydrogen Fuel from Seawater for Mere Pennies
Cutting-Edge Facility Generates Pure Water and Hydrogen Fuel from Seawater for Mere Pennies
 This tiny dev board is packed with features for ambitious makers
This tiny dev board is packed with features for ambitious makers
 Scientists Discover Gel to Regrow Tooth Enamel
Scientists Discover Gel to Regrow Tooth Enamel
 Vitamin C and Dandelion Root Killing Cancer Cells -- as Former CDC Director Calls for COVID-19...
Vitamin C and Dandelion Root Killing Cancer Cells -- as Former CDC Director Calls for COVID-19...
 Galactic Brain: US firm plans space-based data centers, power grid to challenge China
Galactic Brain: US firm plans space-based data centers, power grid to challenge China
Implants made of your blood could repair broken bone
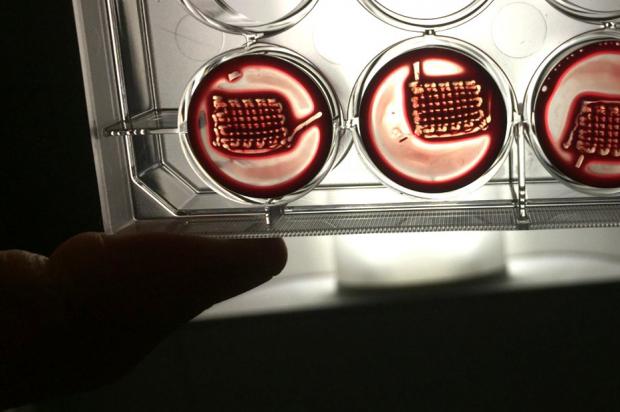
Now scientists at the University of Nottingham have developed a way to improve on the natural process, making implants created from a patient's own blood to regenerate injuries, even repairing bone.
Bodily tissues can heal small cuts or fractures pretty efficiently. It starts with blood forming a solid structure called a regenerative hematoma (RH), a complex microenvironment that summons key cells, molecules and proteins that regenerate the tissue.
For the new study, the Nottingham researchers created an enhanced version of an RH. Rather than making a completely synthetic one from scratch, they used real blood and boosted its healing properties with peptide amphiphiles (PAs) – synthetic proteins that have different regions that are attracted to water and fats. Essentially, the PAs can build better structures for the hematoma, allowing the healing factors and cells that blood summons to work more effectively.
The team demonstrated that the new materials could perform the usual RH functions, such as recruiting healing cells and generating growth factors, while also being easy to assemble and manipulate. These structures can even be 3D printed into whatever shape is needed for any given patient, using samples of their own blood.
The researchers tested the idea in rats, which had sections of bone surgically removed from their skulls. These new RH structures were grown from their own blood and implanted into the gaps, and sure enough, the injuries showed signs of regeneration. After six weeks, those rats that had received the new RH technique showed up to 62% new bone formation, compared to 50% using a commercially available bone substitute. Untreated control rats saw just 30%.
"The possibility to easily and safely turn people's blood into highly regenerative implants is really exciting," said Dr. Cosimo Ligorio, an author of the study. "Blood is practically free and can be easily obtained from patients in relatively high volumes. Our aim is to establish a toolkit that could be easily accessed and used within a clinical setting to rapidly and safely transform patients' blood into rich, accessible, and tunable regenerative implants."



